Unlocking the master checkpoint of cancer immunity
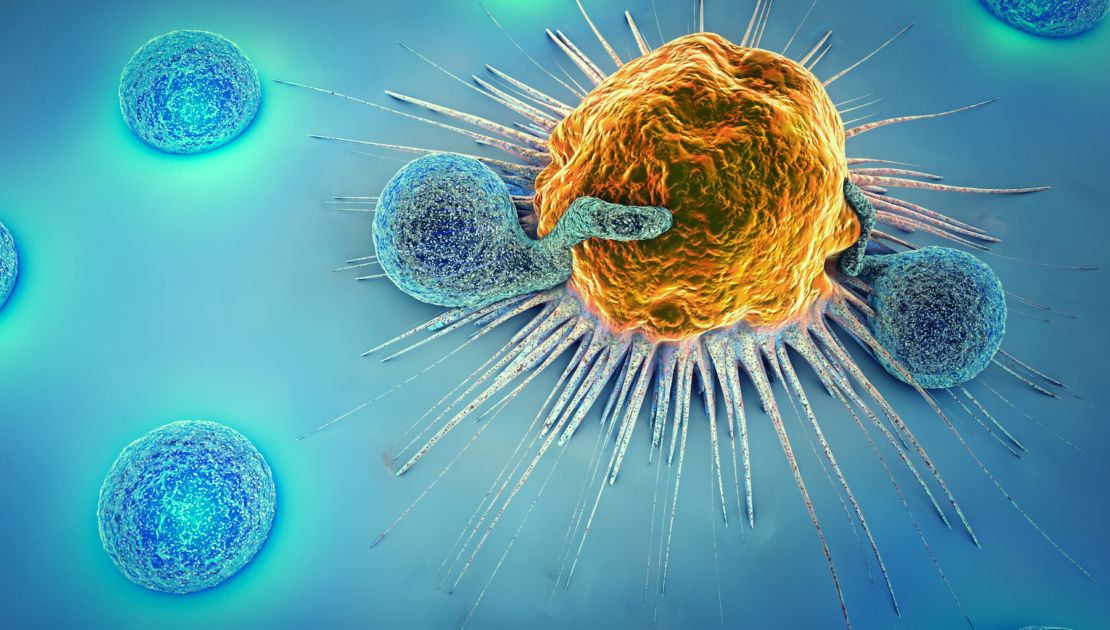
Our knowledge of cancer is growing daily, bringing with it new treatment strategies. As mentioned previously (here) novel immunotherapies are at the forefront of cancer research. The immune activating monoclonal antibodies (mAb) have successfully been established in cancer therapy alongside surgery, radiation, and chemotherapy triggering an increased focus on unleashing brakes on immunity, known as ‘checkpoints’ to awaken anti-cancer immunity. Early efforts were put into enhancing the direct cytotoxic effects on targeted tumor cells. Current mAb products focus on two distinct pathways, PD-1/PD-L1 and CTLA-4, representing immune checkpoints and being inhibitory receptors.
Cytotoxic T lymphocyte antigen-4 (CTLA-4) was the first T cell checkpoint to be identified. In 2011, the FDA approved the first immune-checkpoint blockade therapy, the anti-CTLA-4 mAb Ipilimumab, based on results from a clinical trial in melanoma patients [1]. Multiple drugs blocking these pathways are licenced for use in various cancers, showing particular success in the treatment of melanoma, and lung cancers [2]. The discovery of these therapies resulted in award of the 2018 Nobel Prize for Physiology or Medicine. Although the treatments are used widely, many patients are not able to benefit, relapse or even remain refractory to therapy. A limitation of mAb therapy is that efficacy is dependent on tumor cell expression of the respective target molecules. However, tumors tend sometimes to evolve and change their antigen expression patterns in the course of the disease.
No patient left behind
Despite successes with current checkpoint inhibitors, there are large numbers of ‘non-responders’ and patients who relapse following treatment. This is due to a number of reasons, including alternative brakes on immunity and adaptation of tumors to avoid destruction by newly activated immune cells. Blocking a single immune checkpoint pathway is only successful in some cases as tumors evolve multiple survival mechanisms. There are often many other factors allowing the cancer to survive, meaning that blocking a single checkpoint is simply not enough. One study looking at use of the drugs across the US found that while 40% of patients were eligible for treatment, only 12% showed durable response [3]. Due to these limitations, there is a demand for novel solutions in the field of checkpoint inhibition.
The master checkpoint of cancer immunity
Much interest in the field has come through the discovery of a “master” regulator of checkpoint. The Casitas B-lineage lymphoma proto-oncogene-b or ‘Cbl-b’ protein has been identified as a central determinant of immune cell activation – and even shown to “override” negative antitumor immune regulation by both PD-1 and CTLA-4. The protein is found intracellularly and functions by targeting specific proteins for degradation. This role is known as ‘ubiquitination’ and allows central control over the activity of the immune cells. In addition to T cell-mediated effects, it has been reported that Cbl-b knockout mice have enhanced NK cell-mediated tumor immunity [4]. Targeting, i.e. blocking Cbl-b in cancer immunotherapy offers the opportunity to simultaneously override numerous relevant “checkpoints” [5]. Alongside its position at the heart of the immune activation signalling network, Cbl-b is important due to its expression in different types of immune cells, all of which play a role in controlling tumor growth. Its presence in these cell types means that the protein can be targeted more widely than traditional checkpoints to enhance both innate [6] and adaptive [7] immunity.
A new approach to immune cell therapy
Targeting Cbl-b represents a new age in cancer immunotherapy. Studies in mice have already shown that disrupting the protein can enhance tumor killing [8] and restore the function of previously unresponsive adaptive immune cells [9]. Blocking the central regulator means that the immune cells resist silencing by tumor suppressive signalling through multiple pathways, reducing the risk of tumor resistance and relapse. Developing inhibitors for Cbl-b could provide a revolutionary new solution to awakening anti-tumor responses, providing hope for patients with various tumors.

